Orthopedic Specialist Bruce Steinberg Explains Symptoms and Surgical Techniques for Treating Thumb Arthritis
By Dr. Bruce Steinberg

One of the most common causes of pain when pinching, grasping, torquing (twisting), and lifting with the hand, is arthritis at the base of the thumb. A complex saddle-shaped joint at the base of the thumb allows for movement of the thumb away from the palm. This joint also allows the thumb to pivot and turn so as to meet one or all of the fingers in opposition, which one might visualize as the thumb touching each of the fingertips. This complex function requires that the thumb be strong, flexible, and stable. The forces generated at the thumb base joint are extremely high. In a simple pinching maneuver, the force is 12 times greater at the base of the thumb than it is at the tip of the thumb. A lifetime of use, or trauma, may lead to osteoarthritis of this joint, the trapeziometacarpal joint, which is located between the trapezium and first metacarpal (see figure 1). Even the simplest tasks of daily living such as turning a key, grasping a doorknob, opening a car door, buttoning a shirt, or brushing ones’ teeth, can become impossible when one suffers from trapeziometacarpal joint arthritis. Osteoarthritis of this joint is most commonly seen in middle-aged or postmenopausal women. Female prevalence of this degenerative process is most likely due to greater joint laxity which leads to increased joint incongruity (the two sides of the joint don’t line up smoothly and evenly). Combining joint incongruity with high frequent forces leads to an accelerated degenerative process (osteoarthritis).
A careful clinical examination of the thumb and x-rays will make the diagnosis of osteoarthritis of the trapeziometacarpal joint. There are many treatments for trapeziometacarpal joint arthritis. Rest and non-steroidal anti-inflammatory medications should be the first step. If this fails, the treating physician may wish to try a Medrol Dosepak and consider a custom designed splint for the hand and thumb. An occupational therapist with special splint training is best equipped to make a hand based splint that incorporates the thumb. Unfortunately, most patients have difficulty tolerating the splint since it reduces thumb function considerably by limiting mobility of the trapeziometacarpal joint. Another option is an injection of corticosteroid into the trapeziometacarpal joint. The injection will usually resolve the pain in the early stages of arthritis; advanced stages may have no improvement. If there is no improvement in pain despite the previously described conservative efforts, the next step would be to consider surgical intervention.
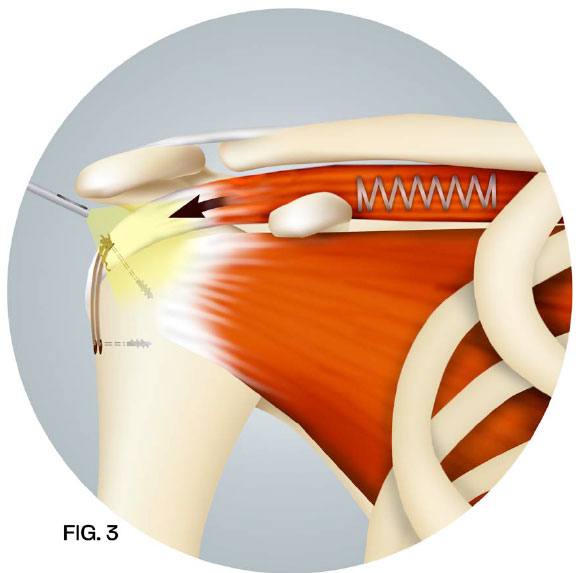
A surgical technique has been developed that is designed to last a lifetime. In this surgery, the arthritis at the base of the thumb is removed (see figure 2). An extra wrist flexor tendon, the flexor carpi radialis tendon, is released in the mid-forearm and placed through the bone at the base of the thumb (see figure 3). It is secured under tension to the base of the thumb by using a suture arising from an anchor. This tendon is then channeled underneath the base of the thumb and weaved back and forth to itself to fill the space created by the removal of the arthritic bone. Because the blood supply to the tendon has not been disrupted, this living joint replacement tissue becomes stronger with time. This surgical procedure takes less than an hour to complete in an outpatient setting. Therapy is started after 10 days and the protective splint is worn for 6 weeks following surgery. Long-term follow up studies have shown 95% of patients experiencing excellent relief of pain while also restoring thumb function.


Should Pain and Rotator Cuff Surgery Video
Click the last button on the player to enlarge the video.
You will need Adobe Flash to watch the video
Orthopedic Specialist Dr. Bruce Steinberg Uses Advanced Techniques to Treat Shoulder Pain and Perform Rotator Cuff Surgery
By Bruce Steinberg, M.D.
Pain, weakness, clicking and popping in the shoulder area are some of the common symptoms of rotator cuff tears. Tears of the rotator cuff can occur in individuals of all ages.

A single, heavy lifting event is the usual cause for a younger patient (under 40years), while older patients (greater than 60), may injure the rotator cuff with minimal force. As we get older, the rotator cuff may weaken and fray secondary to bone spurs that form within the shoulder (Figure 1).
Once the rotator cuff tear occurs, the muscle pulls on the tendon, retracting it away from its insertion and propagating the tear through the remaining tendon (Figure 2).

Minimally invasive techniques have been developed to repair the rotator cuff and remove bone spurs. A fiberoptic camera is introduced into the shoulder joint through a small puncture (portal). Through a second working portal, the surgeon uses instruments to place anchors into the bone.
Sutures arising from the anchors are weaved through the rotator cuff tendon and special knots are tied that cinch the tendon back to its insertion. Bone spurs within the shoulder are removed with a small bur (Figure 3).
This advanced technique has proven to be an extremely effective option for repairing rotator cuff tears while also minimizing recovery time for patients.
For enlarged images download Pdf »
To Perform His Shoulder Surgery, Dr. Koster Selected Dr. Steinberg, A Top Upper Extremities Surgeon in US
Patient Testimonial: Left Shoulder Fracture & Right Biceps Muscle Rupture / Repair of Proximal Humerus Fracture & Repair of Distal Biceps
When you are unable to use either of your arms, it is the little things that haunt you. Kenneth Koster, M.D., a retired cardiothoracic surgeon, learned this during his recovery from a fall in which he sustained serious injury. “Simple activities assume gigantic proportion when you can’t move your arms. You ask yourself, ‘Is it worth the effort?’ Getting up out of a chair or trying to pick something up from the floor become monumental tasks.” Clearly, Dr. Koster is a man of great determination and self-discipline as is evidenced by his renowned medical career and multiple other interests of which he has been involved over the years. Upon retiring from a career in cardiothoracic surgery, he has had the good fortune to pursue his passion for painting. In fact, it was while leaving his art studio in Chicago that he fell, and in trying to catch himself, severely injured both of his upper extremities.
“I tripped and fell down a flight of stairs and ended up inverted on the floor. The early moments are a blur although I do remember making an assessment of what was working and what was not. I could move my right arm some, but the left arm was gone.” Through a series of events, Dr. Koster was evaluated and provided initial treatment by a specialist in orthopedic trauma in the Chicago area, but ultimately Dr. Koster decided to return to Jacksonville.
“My wife told me that I really needed to come home. I left Chicago not out of a lack of confidence in the people at Northwestern, but with a growing realization of how badly I was injured and the prospect of a long, long recovery.” He contacted Bruce Steinberg, M.D., specialist in upper extremities. “The fact that I knew Dr Steinberg's reputation made the decision to come home for treatment easy.” Dr. Koster continues to say that some physicians shy away from treating other doctors, especially very difficult cases. “I was a mess, but Dr. Steinberg did not blink. He was determined to do all that he could for me.”
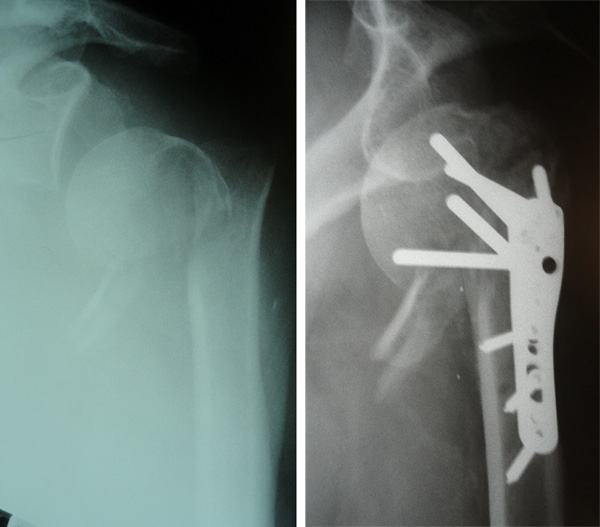
Through examination and testing, Dr. Steinberg diagnosed Dr. Koster with a displaced, comminuted proximal humerus fracture of his left upper extremity and a distal biceps rupture with retraction of his right upper extremity. The required surgical repair was somewhat complicated because a month had passed since the accident. After much discussion of options, Dr. Steinberg, with Dr. Steven Crenshaw, performed both a left side repair of the proximal humerus fracture and a right side distal biceps repair.
Dr. Koster shares that the period immediately following his surgery was especially difficult due to his need for total reliance on others. During this time, his wife cared for his every need. “It was a low point, and it certainly put many things in perspective.” He knew, however, that his recovery was a matter of several components coming together: expert surgical skill applied to extreme injury, time for healing, and then, when his body was ready, a rigorous course of physical therapy, of which he would need to totally commit. About five months after his surgery, Dr. Koster realized that certain motions of his left arm during therapy “hurt beyond all others.” Dr. Steinberg determined that further surgical repair was required and thus Dr. Koster underwent a left shoulder removal of some of the hardware installed during the initial surgery.
While his recovery has been long, Dr. Koster is mindful that due to the extent of his injuries, this is not surprising. He has dedicated himself to a regimen of therapy, with occupational JOI physical therapist, in particular Christian Prado (MOTR-L), and also at home, where he has created a circuit of stretching bands. The combination of activities has helped his range of motion and strength. Dr. Koster is happy to report that recently he has noted “a real turn for the better” in terms of regained strength in his arms. “While I certainly have not enjoyed this experience, I do appreciate what I learned on a personal level. After my fall, I realized fairly quickly that expert medical care would be essential. Dr. Steinberg is a perfectionist who insists on doing things correctly. This has certainly been validated by my experience.”
Understanding Carpal Tunnel Syndrome

By Bruce Steinberg, M.D.
The most common cause of numbness and tingling of the upper extremity is carpal tunnel syndrome. Symptoms may also include sharp, piercing pain that radiates from the wrist to the fingertips, and/or from the wrist to the shoulder. When these symptoms occur, individuals will often stop what they are doing, and may shake their hands in order to obtain relief. This pain may occur while performing simple activities such as driving and typing. The symptoms of carpal tunnel syndrome are very similar to those experienced when sitting for a long period of time, such as in a movie theatre. When one stands up, the foot feels as if it is “asleep.” A sensation of “pins and needles” occurs within the foot, but by walking and shaking the foot, these symptoms go away. This condition occurs from compression or squeezing of the sciatic nerve along the back of the thigh. In the upper extremity, carpal tunnel syndrome occurs from compression or squeezing of the median nerve at the level of the wrist. The carpal tunnel is a narrow, rigid canal formed by a thick ligament (transverse carpal ligament) on one side, and the bones of the wrist on the other (Fig. 1).
The carpal tunnel houses the median nerve and the tendons of the fingers. Swelling within this canal leads to the squeezing of the nerve as it goes through this confined space. Electrochemical impulses travel from the neck to the fingertips, much like a garden hose transporting water. When the nerve is squeezed like the hose being kinked, the symptoms of pain, numbness, tingling, and weakness occur due to the decreased flow of the electrochemical impulses. In addition to having compression of the nerve at the level of the wrist, an individual may also have compression of the nerve at the neck from arthritis or a herniated cervical disk. The nerve, in this situation, is like a hose with kinks in two places, both decreasing flow. Metabolic conditions such as diabetes, thyroid disease, kidney disease, and vascular disease, may affect the amount of electrochemical impulses that travel down the nerve similar to a faucet on low flow (Diag. 1).

The combination of a low faucet flow and kinking of the hose/nerve in more than one area can compound the symptoms. When evaluating for carpal tunnel syndrome, other conditions such as cervical spine disease and metabolic causes such as diabetes, etc., must be ruled out. A thorough history and careful clinical examination from the neck to the fingertips and sometimes an electrophysiological test (EMG/NCV) will help confirm the diagnosis. Once the diagnosis of carpal tunnel syndrome has been established, the treatment is aimed at taking away the compression of the nerve at the level of the wrist. A simple over-the-counter wrist splint positioned to extend the wrist decreases the kinking of the median nerve. Anti-inflammatory medications such as Motrin and Aleve may also be helpful by decreasing the swelling of the tendons within the carpal canal. When these remedies fail, an injection of cortisone into the carpal tunnel combined with a splint, can significantly diminish the swelling leading to decreased compression of the nerve and thus resolve symptoms. If these conservative treatments fail to decompress the nerve, the canal space can be made larger. Unfortunately, there are no manipulations or devices that will expand the rigid carpal tunnel canal structure.
Surgery is aimed at opening the thick transverse carpal ligament that forms the roof of the canal, giving more room for the median nerve. By opening the transverse carpal ligament, the kink of the nerve is removed and the electrochemical impulses can now flow more normally. The pain, numbness, tingling, and weakness can resolve if the nerve has not been significantly damaged by long-standing compression.
Surgical intervention for carpal tunnel syndrome has significantly progressed. The old technique of an open carpal tunnel release creates an incision within the sensitive palm of the hand. While this approach takes away the kink of the nerve by opening the transverse carpal ligament, the downside is a tender, painful palm. This drawback has been overcome by using an endoscopic device which allows the operation to be done through a ¼ inch incision site away from the palm at the wrist crease.
 The median nerve is directly visualized and therefore the contents of the carpal tunnel can be safely decompressed by releasing the transverse carpal ligament (Fig. 2). While this operation is more technically demanding than the open carpal tunnel procedure, with training and experience, this surgery is safer and leads to excellent relief of the symptoms while allowing faster return to full activity.
The median nerve is directly visualized and therefore the contents of the carpal tunnel can be safely decompressed by releasing the transverse carpal ligament (Fig. 2). While this operation is more technically demanding than the open carpal tunnel procedure, with training and experience, this surgery is safer and leads to excellent relief of the symptoms while allowing faster return to full activity.
For enlarged images download Pdf »
To learn more about endoscopic carpal tunnel release


